Disease of the Month – Myocardial infarction (MI)
Shots:
-
Myocardial infarction (MI), colloquially known as a heart attack, occurs when blood flow to the heart is severely reduced or blocked, causing tissue damage or mortality due to lack of oxygen
-
PharmaShots' Disease of the Month report aims to familiarize the general population with conditions impacting communities worldwide. The report outlines disease characteristics, types, symptoms, diagnosis, treatments, epidemiology, market size, clinical trial analysis, patient advocacy groups (PAGs), and heart-touching patient stories
-
For a detailed Myocardial infarction landscape, analysis, and tailored insights contact our experts at connect@pharmashots.com

Did you know that about one in five heart attacks are silent? Every 40 seconds, one heart attack is reported in the US. Sedentary lifestyles attributed to a lack of physical activities and unhealthy food habits (high cholesterol) lead to cholesterol build-up in coronary arteries and a condition called atherosclerosis. With this illuminating guide, let's understand the silent devil called Myocardial Infarction (MI) that poses grave concerns to mankind.

MI can be classified into 5 types based on cause and circumstances:[1]
Type 1: Spontaneous MI results from ischemia (lack of blood supply to a part of the body) from a primary coronary event (e.g., plaque rupture, erosion, or fissuring; coronary dissection)
Type 2: Ischemia resulting from increased oxygen demand (e.g., hypertension) or decreased supply (e.g., coronary artery spasm or embolism, arrhythmia, hypotension).
Type 3: Related to sudden unexpected cardiac death
Type 4: There are 2 subtypes:
- Type 4a: Associated with percutaneous coronary intervention, showing MI signs and cTn values > 5 × 99th percentile upper reference limit (URL)
- Type 4b: Associated with stent thrombosis
Type 5: Associated with coronary artery bypass grafting, showing MI signs and cTn values > 10 × 99th percentile upper reference limit (URL)
MI can be caused by various conditions and factors, including: [2]
-
Coronary Artery Disease (CAD) and Atherosclerosis
-
Coronary Artery Spasm
-
Rare medical conditions causing unusual narrowing of blood vessels
-
Trauma causing tears or ruptures in the coronary arteries
-
An obstruction, like a blood clot or air bubble (embolism) that blocks a coronary artery
-
Eating disorders
-
Anomalous Coronary Arteries
-
Genetics

Some common MI symptoms include: [2]
-
Angina
-
Trouble breathing
-
Insomnia
-
Nausea
-
Heart palpitations
-
Anxiety
-
Dizziness

MI is usually diagnosed in the emergency room. Providers will check the pulse, oxygen levels, and blood pressure, as well as the sound of the heart and the lungs. [3]
A healthcare provider will diagnose a heart attack using:
-
Blood Tests: A reliable way to diagnose a heart attack is by checking for cardiac troponin in the blood, as it appears when heart muscle cells are damaged
-
Electrocardiogram (EKG or ECG): This test is one of the first in the ER for heart attack symptoms, as it helps detect injury and rhythm abnormalities through the heart's electrical signals
-
Echocardiogram: It uses ultrasound to create a picture of your heart, showing how well it’s squeezing and how the valves are functioning
-
Coronary Angiogram or Heart Catheterization: This procedure uses X-rays and contrast dye to depict heart blood vessels and identify blockages
-
Heart CT Scan: This scan provides a detailed image of the heart and blood vessels to detect narrowing or hardening of the coronary arteries
-
Heart MRI: This test uses a magnetic field and computer to create an image of the heart, showing blood flow issues in the arteries
-
Exercise Stress Test: This test uses an ECG, echocardiogram, or nuclear scans during physical activity to check if the heart is getting enough blood flow
-
Nuclear Heart Scans: These scans use a radioactive dye and CT to identify areas of the heart with reduced blood flow or damage, including SPECT or PET scans

Treating a heart attack involves restoring blood flow to the heart quickly, using methods such as medication or surgery. Treatment includes: [3]
Supplementary oxygen: People with breathing issues or low oxygen levels often receive supplementary oxygen through a tube or mask, improving blood oxygen and reducing strain on the heart.
Medications: Several medications such as Anti-clotting medications, Nitroglycerin, Thrombolytic (clot-busting) medications, Antiarrhythmia medications, Pain medications, Beta-blockers, Antihypertensives, and Statins are used to manage MI
Percutaneous Coronary Intervention: Providers restore blood flow to the heart through percutaneous coronary intervention (PCI) or angioplasty, using a catheter to open the artery. The quicker this is done, the better the outcome. "Door-to-balloon time" is a metric used by the providers to measure how fast PCI is performed after arrival in the ER. A stent may be placed to keep the artery open and prevent future blockages.
Coronary Artery Bypass Grafting: Severe coronary artery blockages may require coronary artery bypass grafting (CABG), or bypass surgery. This procedure uses a blood vessel from another part of your body to create a detour, bypassing blocked arteries and delivering blood to the heart.

Prevalence: The global prevalence of MI in individuals less than 60 & more than 60 years yrs. were found 3.8% & 9.5%, respectively [4]
Gender: MI was found to be 5 times more prevalent in males

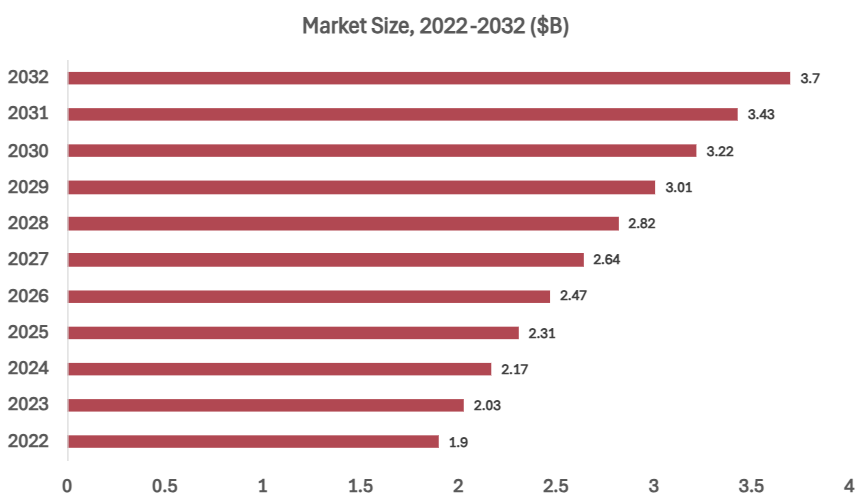
In 2022, the global MI treatment market was valued at $1.9B and is projected to reach $3.7B by 2032, growing at a CAGR of 6.8% from 2023 to 2032 [5]

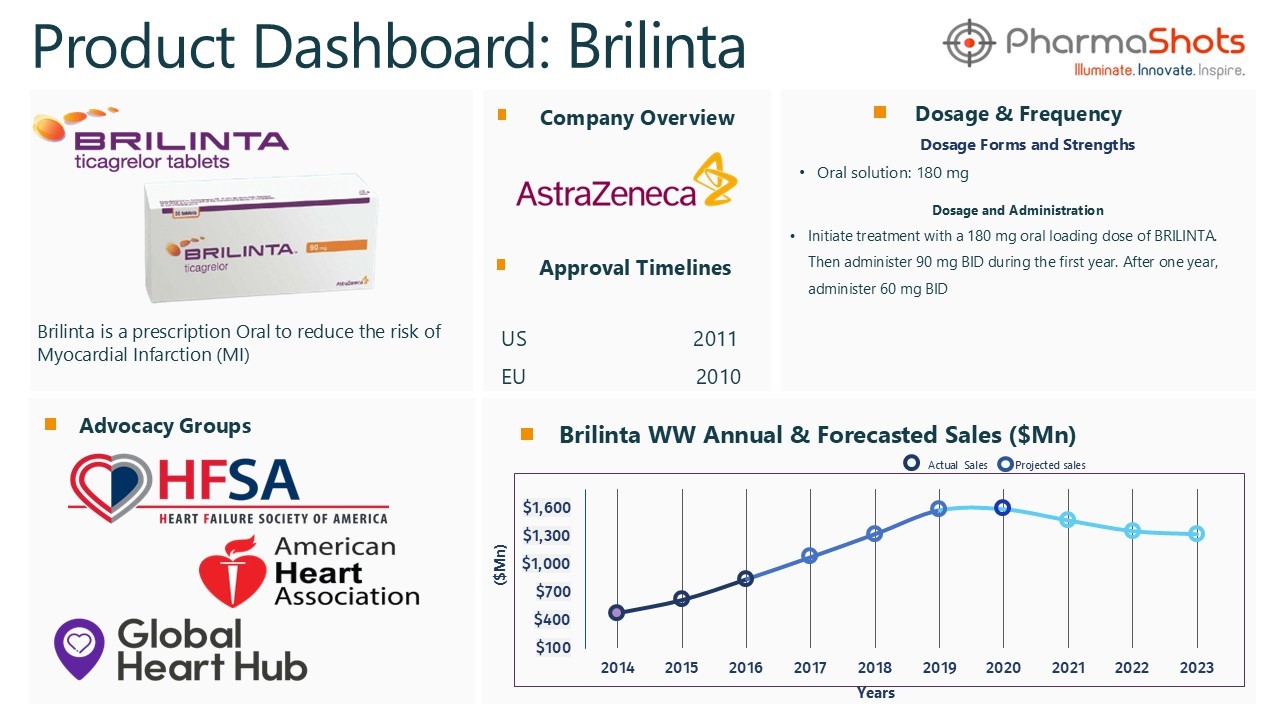
Brilinta (ticagrelor) is indicated to reduce the risk of Myocardial Infarction (MI) and is marketed under the brand name Brilique in the EU [6]

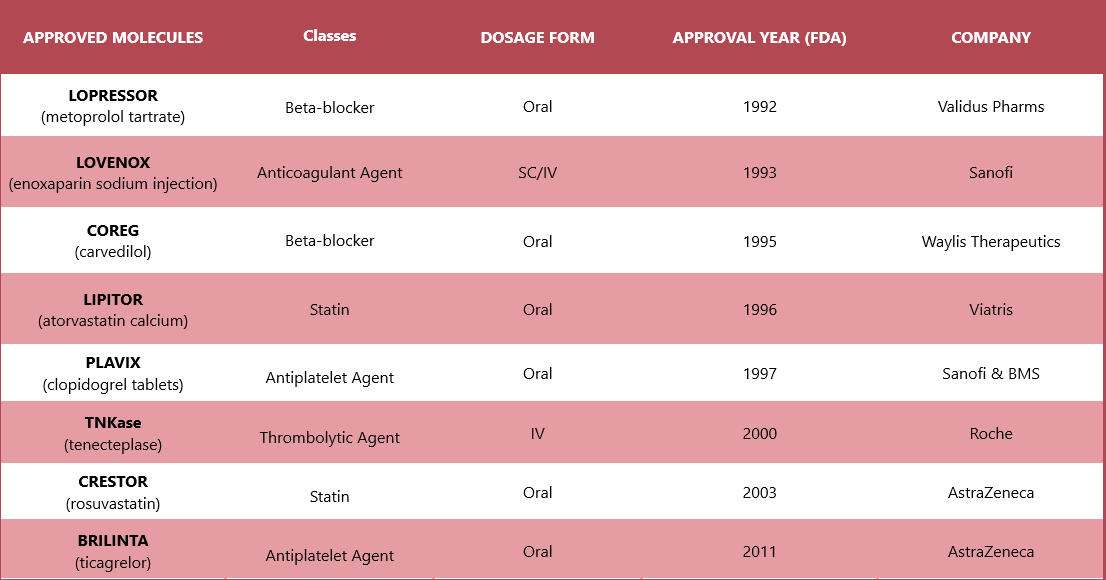
Approved therapies include Lopressor (Alembic Pharmaceuticals), Lovenox (Sanofi), Coreg (Waylis Therapeutics), Lipitor (Viatris), Plavix (Sanofi & BMS), TNKase (Roche), Crestor (AstraZeneca), and Brilinta (AstraZeneca)

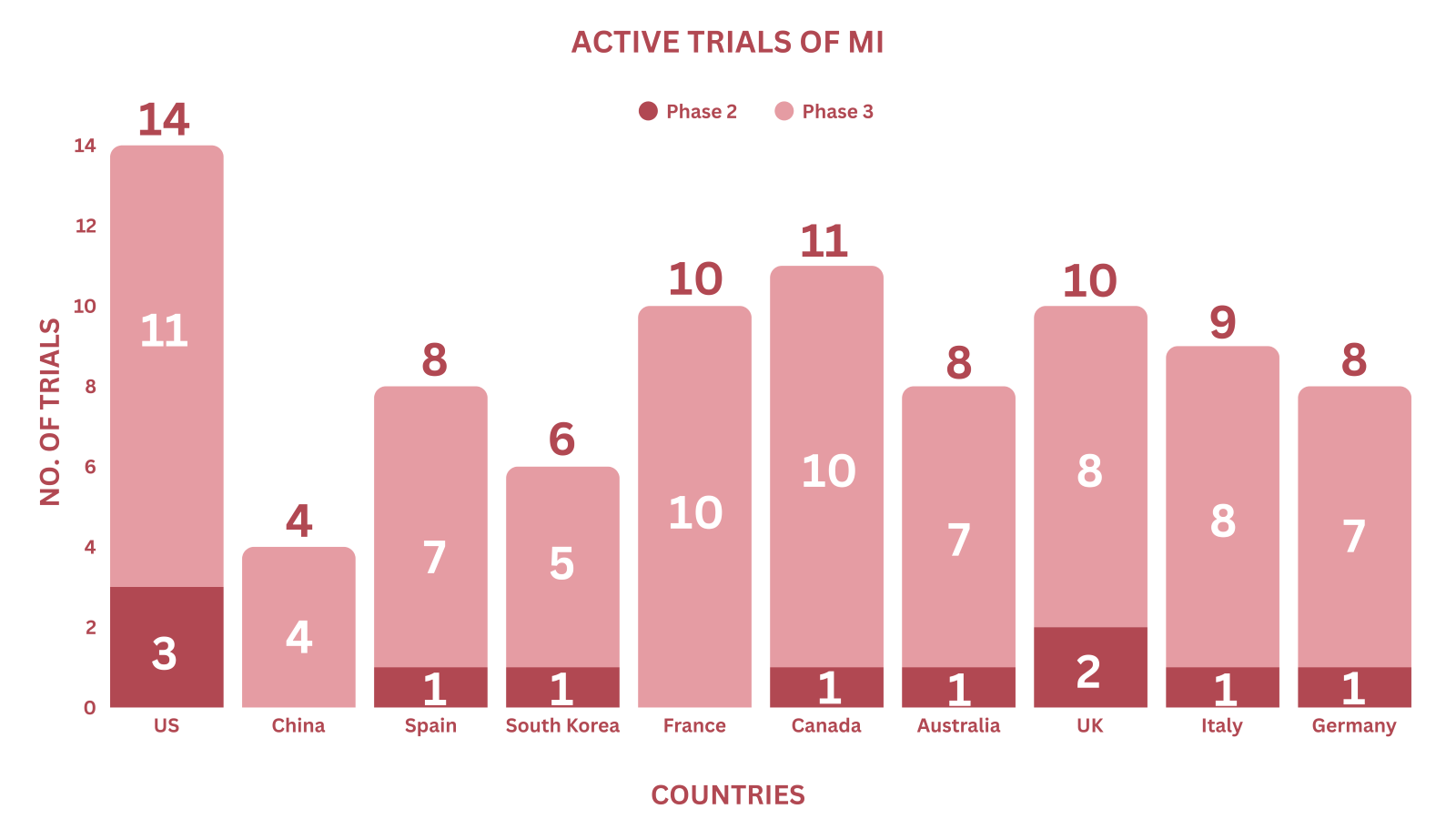
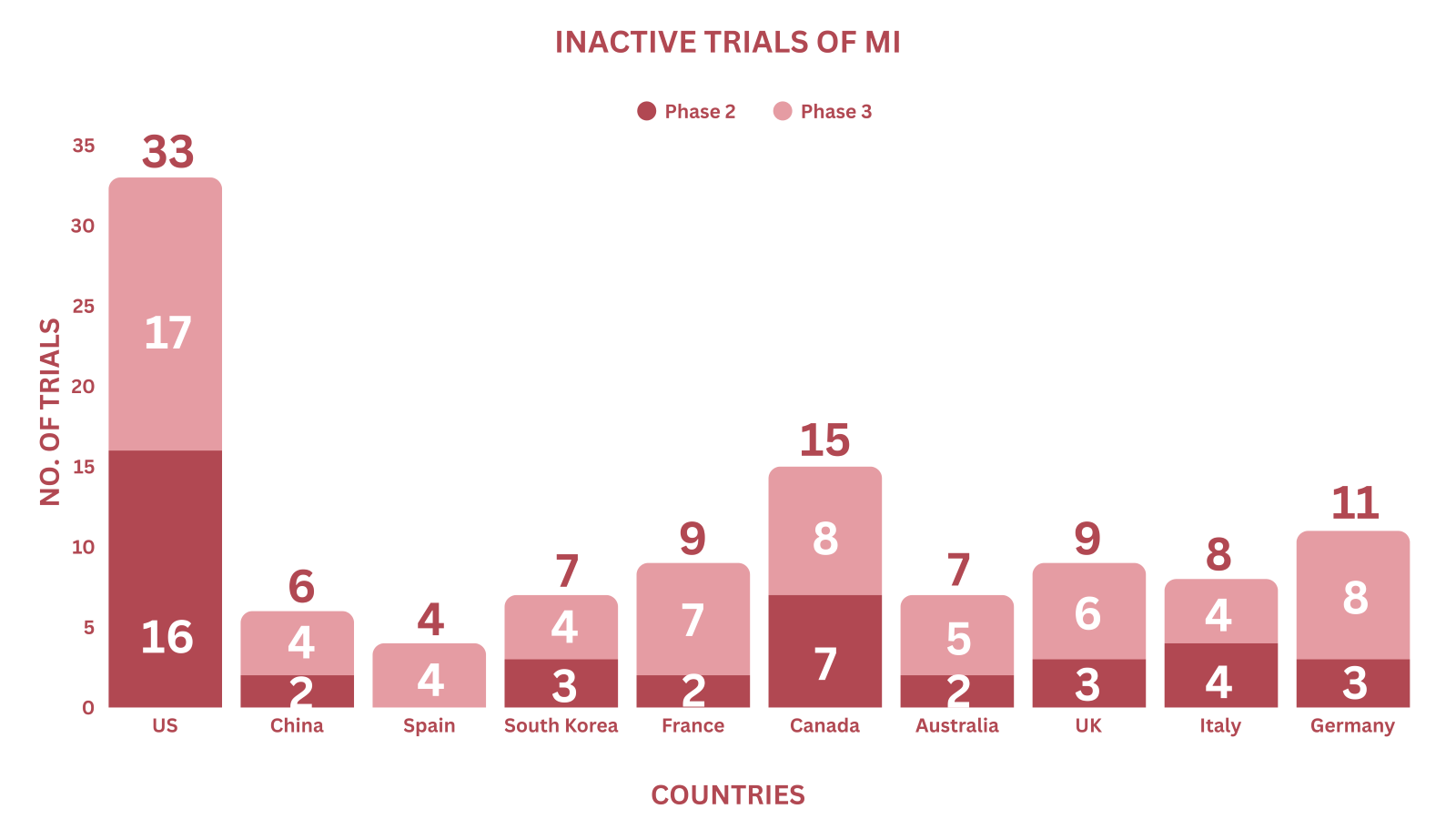
Active & Inactive Trials of P-III are concentrated in the US, followed by Spain, Australia, and Italy. Data were extracted on Apr 15, 2025 [7]

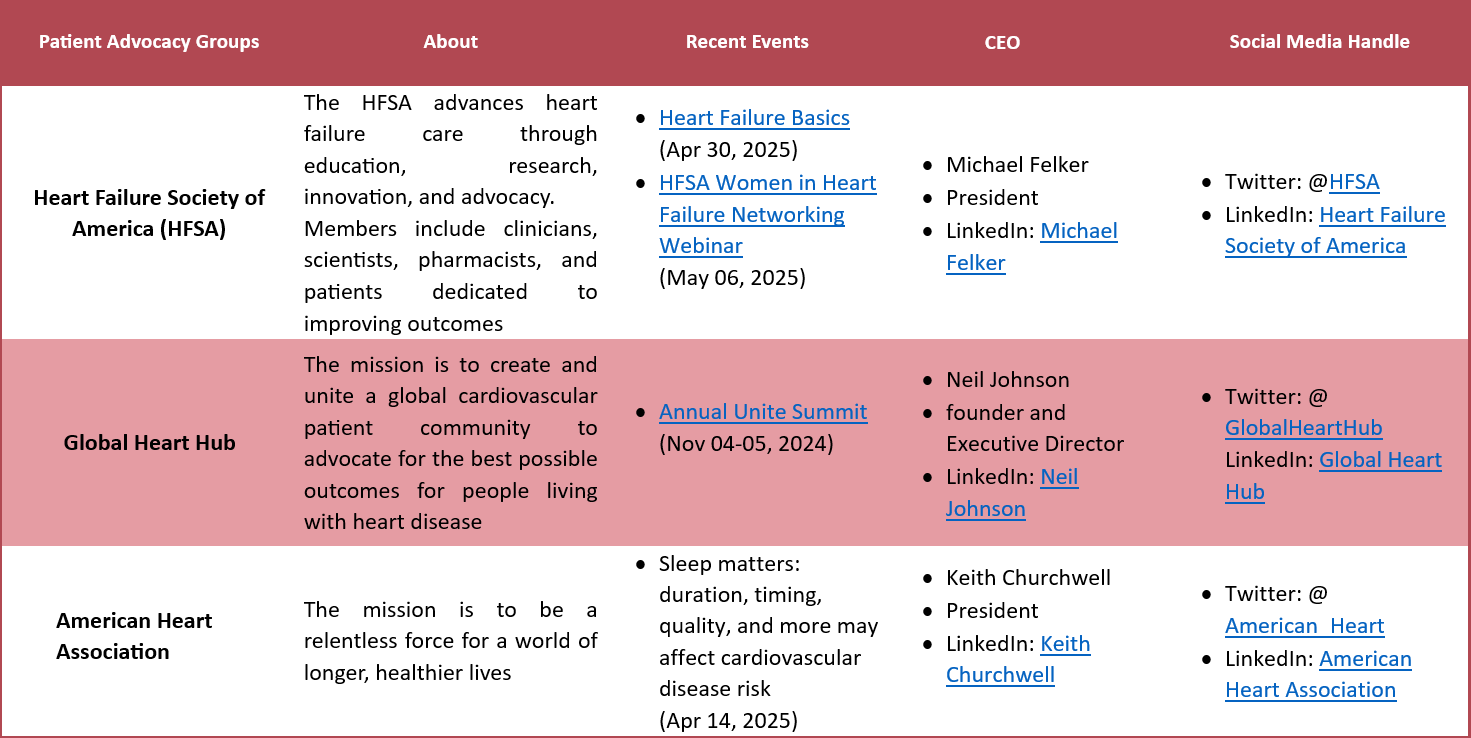
Several patient advocacy groups are dedicated to supporting individuals with MI and improving their quality of life.

1. Debbie Siddons [8]
It was the usual rush in the Siddons household as Debbie raced around getting her four children ready for school. But as she walked into the living room to summon her eldest, she was suddenly stopped by a sharp pain in her chest.
"My heart was racing, the pain was awful and I had pins and needles in my lower jaw and down both arms," she says. "I sat down on the sofa hoping the pain would stop, but it didn't. I knew something was very wrong. I was on my own with the kids, so I got my eldest to bring me the phone. I called my mother-in-law and my father, and told them I didn't feel very well. My dad was over in 10 minutes. He took one look at me and called an ambulance."
In the ambulance, paramedics gave Debbie an electrocardiogram (ECG) to test the electrical activity in her heart. She was then given an aspirin to chew. Once she got to the hospital, doctors gave her a drug to dissolve any clots in her blood that might have caused the heart attack.
"I knew it was serious, but I didn't guess how serious," she says. "When I got to the hospital, it was madness. Everyone was rushing around, hooking me up to machines. It didn't take the doctor long to tell me I'd had a heart attack. It didn't quite sink in until my mother-in-law got to the hospital and I had to tell her what had happened to me."
Debbie stayed in hospital for a week. On the sixth day, she began to experience pins and needles in her left arm. Doctors were concerned that she might be having another heart attack. As a precaution, she was given another ECG and sent for an angiogram procedure that checks the arteries for blockages. The angiogram was clear, and Debbie didn't have another attack. The cause of her original attack is still unknown.
Back at home, she realised how much the experience had shaken her. "I was frightened to do anything. I was nervous about going up the stairs and I was too scared to pick up my 18-month-old daughter in case I had another heart attack," she says.
"Then I was sent for rehabilitation, which really helped. We learned about healthy eating and exercise, but a big part of it was finding the confidence to carry on with our lives. The nurses reassured me that I could live a perfectly normal life again and they were right. By the end of the six-week course, I'd got my confidence back."
Debbie sees a consultant once a year and hasn't had another heart attack. "It was a very frightening experience, but I came through it," she says. "I'd urge anyone who's had a heart attack to make the most of rehabilitation and use all the help they can get. It certainly helped me to move on.
2. Jennifer Cooper Cheak [9]
Jennifer Cooper Cheak was playing with her 3-week-old baby and son when she started to feel tightness and pressure in her chest. A few minutes later, the 32-year-old experienced a heart attack and was rushed to a local hospital in Waco, Texas.
The Waco hospital said she had arrived unresponsive and estimated about 40 minutes downtime. The team knew she needed a miracle and made the decision to send her where that could be made into a possibility – the Larry D. Johnson Heart & Vascular Institute at Memorial Hermann-Texas Medical Center.
“When Jennifer came into our hospital, her blood results were very bad,” said Isabel Ponce, RN, BSN, cardiovascular intensive care unit (CVICU). “We knew we had a difficult journey ahead of us.” Cheak arrived via LifeFlight® and was immediately taken to the Cardiac Cath Lab. It was at this time that Pranav Loyalka, MD, associate chief of the medical division, Larry D. Johnson Heart & Vascular Institute, told the patient care team, “She’s young and she’s a mother. She has a 3-year-old at home and had her second baby three weeks ago. We are going to do everything possible to help her. Do we all understand?”
Ponce said it was at this moment when the procedure room grew quiet and an unspoken unity was instilled in the team, signaling that they were about to take part in a breakthrough.
“It really hit home for me because my sister has two beautiful children and I couldn’t imagine them living without their mom. I knew that I had to fight for Cheak and do whatever it took to keep her alive,” said Ponce.
Collaborating with fellow physicians at the Center for Advanced Heart Failure at Larry D. Johnson Heart & Vascular Institute, Dr. Loyalka, associate professor of internal medicine at The University of Texas Health Science Center at Houston (UTHealth) Medical School, decided to intubate and insert a Tandem Heart.
“Day one was trying to keep her alive. Morning of day two, her labs were better but she still hadn’t woken up,” said Ponce. “By the end of day two, she opened her eyes and was looking around. Day three she began following commands.”
Over the weekend, Dr. Loyalka removed the balloon pump that was placed earlier that weekend because he found her heart was beating on its own. “When we performed the first echocardiogram (echo), her heart was functioning at 10%. After we removed the balloon pump and performed the second echo, her heart was up to 30%,” said Dr. Loyalka.
Cheak slowly started showing signs of improvement; her family and caregivers were determined to get her better. Ponce said, “Her family was incredibly supportive and there for her every minute of the day speaking words of encouragement. They also fully trusted me and the care team, remaining actively involved in the plan of care.”
Cheak said, “Isabel was a fantastic nurse and I don’t know what I would have done without her. She motivated me to not give up and stay strong for my kids and family. I also couldn’t speak more highly of the physician team, especially Dr. Loyalka. He is a king among kings in my book! He gave me a second chance at life.”
As a result of the great care from the physicians, nurses and all the caregivers at the Institute, Cheak has made a full recovery and is able to stay at home with her husband and care for their newborn boy and son
References
- MSD Manual
- NHS
- Cleveland Clinic
- BMC
- Spherical Insights
- Brilinta PI
- CT.GOV
- Patient story 1
- Patient story 2
Related Post: Disease of the Month – Lennox-Gastaut syndrome (LGS)
Tags

A passionate content writer with expertise in delivering high-quality and engaging content, Dipanshu is a keen reader and a versatile writer. Dipanshu dedicatedly covers news ranging from biopharma, life sciences, biotech, and MedTech to diagnostics and animal health companies, FDA, EMA, and biosimilar approvals. He can be contacted at connect@pharmashots.com